|
Parkinson's
Disease is due to the insufficient formation and action of dopamine. Human
beings have always had the potential for insufficient dopamine. So
although Parkinson's Disease has increased in its prevalence over time, it
must have existed to some extent for as long as human beings. There are
references to Parkinson's Disease symptoms throughout history.
Ancient HISTORY
 An ancient
civilisation in India practiced their medical doctrine called Ayurveda.
Ayurveda is claimed to be a divine revelation of the ancient Indian
creator God Lord Brahma.
It describes
the symptoms of Parkinson's Disease, which they called Kampavata as far back as
5000 B.C.. To treat Kampavata, they used a tropical legume called Mucuna Pruriens,
which is a natural source of
therapeutic quantities of L-dopa. Mucuna pruriens is the oldest known
method of treating Parkinson's Disease, and is still being
used today. An ancient
civilisation in India practiced their medical doctrine called Ayurveda.
Ayurveda is claimed to be a divine revelation of the ancient Indian
creator God Lord Brahma.
It describes
the symptoms of Parkinson's Disease, which they called Kampavata as far back as
5000 B.C.. To treat Kampavata, they used a tropical legume called Mucuna Pruriens,
which is a natural source of
therapeutic quantities of L-dopa. Mucuna pruriens is the oldest known
method of treating Parkinson's Disease, and is still being
used today.
 The Huang di nei
jing su wen (often known as the Su wen), is the oldest existing Chinese
medical text. It was written in around 500 B.C..
It is composed of two texts
each of eighty one chapters or treatises in a question and answer format
between the mythical Huang di (Yellow
Emperor) and his ministers.
The first text, the Suwen, also
known as Plain Questions, covers the theoretical foundation of
Chinese Medicine, diagnosis methods and
treatment methods.
It also describes the symptoms of Parkinson�s Disease. The Huang di nei
jing su wen (often known as the Su wen), is the oldest existing Chinese
medical text. It was written in around 500 B.C..
It is composed of two texts
each of eighty one chapters or treatises in a question and answer format
between the mythical Huang di (Yellow
Emperor) and his ministers.
The first text, the Suwen, also
known as Plain Questions, covers the theoretical foundation of
Chinese Medicine, diagnosis methods and
treatment methods.
It also describes the symptoms of Parkinson�s Disease.
 It
is claimed that there are references to the symptoms of Parkinson�s
Disease in both the old and new testaments of the Bible. Often cited as
possible references to Parkinsonism is the following depiction of old age
in the Old Testament : "When the guardians of the house tremble, and the
strong men are bent" (Ecclesiastes 12 : 3), and the following description
in the New Testament "There was a woman who for eighteen years had been
crippled by a spirit.....bent and completely incapable of standing erect"
(Luke 13:11). It
is claimed that there are references to the symptoms of Parkinson�s
Disease in both the old and new testaments of the Bible. Often cited as
possible references to Parkinsonism is the following depiction of old age
in the Old Testament : "When the guardians of the house tremble, and the
strong men are bent" (Ecclesiastes 12 : 3), and the following description
in the New Testament "There was a woman who for eighteen years had been
crippled by a spirit.....bent and completely incapable of standing erect"
(Luke 13:11).
ANCIENT GREEKS
 In
the Illiad, which, along with the Odyssey are claimed to have been written
by the ancient Greek author Homer in the eighth century B.C., the septuagenarian King Nestor
describes symptoms that appear to be those of Parkinson's Disease. King
Nestor
remarks that, despite the fact he still partakes of the armed struggle, he
can no longer compete in athletic contests. He wrote that : my limbs are no longer
steady, my friend, nor my feet, neither do my arms, as they once did,
swing light from my shoulders. In
the Illiad, which, along with the Odyssey are claimed to have been written
by the ancient Greek author Homer in the eighth century B.C., the septuagenarian King Nestor
describes symptoms that appear to be those of Parkinson's Disease. King
Nestor
remarks that, despite the fact he still partakes of the armed struggle, he
can no longer compete in athletic contests. He wrote that : my limbs are no longer
steady, my friend, nor my feet, neither do my arms, as they once did,
swing light from my shoulders.
 Erasistratus
of Ceos (310BC- 250BC) was a Greek anatomist and royal physician under
Seleucus I Nicator of Syria. Along with fellow Greek Philosopher
Herophilus, he founded a school of
anatomy in
Alexandria. Caelius Aurelianus wrote that Erasistratus of Ceos appeared to be describing the freezing that occurs in
Parkinson's Disease when he termed paradoxos a type of paralysis in which
a person walking along must suddenly stop and cannot go on, but after a
while can walk again. Erasistratus
of Ceos (310BC- 250BC) was a Greek anatomist and royal physician under
Seleucus I Nicator of Syria. Along with fellow Greek Philosopher
Herophilus, he founded a school of
anatomy in
Alexandria. Caelius Aurelianus wrote that Erasistratus of Ceos appeared to be describing the freezing that occurs in
Parkinson's Disease when he termed paradoxos a type of paralysis in which
a person walking along must suddenly stop and cannot go on, but after a
while can walk again.
ANCIENT ROME
 Aulus
Cornelius Celsus (c25BC-c50AD), although apparently not a physician
himself, compiled an encyclopedia entitled De artibus (25AD-35AD) that
included De medicina octo libri (The Eight Books of Medicine).
He advised
against administering those who suffered tremor of the sinews with emetics
or drugs that promoted urination, and also against baths and dry sweating.
Fine
tremor was distinguished from a coarser shaking, which was independent of
voluntary motion. So it resembled resting tremor. It could be alleviated
by the application of heat and by bloodletting. Aulus
Cornelius Celsus (c25BC-c50AD), although apparently not a physician
himself, compiled an encyclopedia entitled De artibus (25AD-35AD) that
included De medicina octo libri (The Eight Books of Medicine).
He advised
against administering those who suffered tremor of the sinews with emetics
or drugs that promoted urination, and also against baths and dry sweating.
Fine
tremor was distinguished from a coarser shaking, which was independent of
voluntary motion. So it resembled resting tremor. It could be alleviated
by the application of heat and by bloodletting.
 Pedanius
Dioscorides (c40-c90)
was an ancient
Greek
physician,
pharmacologist and
botanist from Anazarbus,
Cilicia,
Asia Minor, who practised in
ancient Rome during the time of
Nero. Dioscorides is famous for writing
De
Materia Medica, which is a precursor to
all modern
pharmacopeias, and is one of the most
influential herbal books in history. Dioskorides wrote that beaver
testes, prepared with vinegar and roses was helpful not only for the "lethargicall"
but was also good for tremblings and convulsions, and for all diseases of
the Nerves, being either drank or anointed on, and that it had a warming
faculty. Pedanius
Dioscorides (c40-c90)
was an ancient
Greek
physician,
pharmacologist and
botanist from Anazarbus,
Cilicia,
Asia Minor, who practised in
ancient Rome during the time of
Nero. Dioscorides is famous for writing
De
Materia Medica, which is a precursor to
all modern
pharmacopeias, and is one of the most
influential herbal books in history. Dioskorides wrote that beaver
testes, prepared with vinegar and roses was helpful not only for the "lethargicall"
but was also good for tremblings and convulsions, and for all diseases of
the Nerves, being either drank or anointed on, and that it had a warming
faculty.
 Symptoms of Parkinson�s Disease were described by the ancient Greek
physician Galen (129-200) who worked in ancient Rome. He wrote of tremors
of the hand at rest.
He wrote extensively on disorders of
motor function, including
the book On tremor, palpitation, convulsion and
shivering. He distinguished between forms of shaking of the limb on the
basis of origin and appearance. The aged, he noted, exhibited tremor
because of a decline in their power to control motion of
their limbs. The key to overcoming tremor was to abolish the proximal
cause, but for the aged, this was impractical. Symptoms of Parkinson�s Disease were described by the ancient Greek
physician Galen (129-200) who worked in ancient Rome. He wrote of tremors
of the hand at rest.
He wrote extensively on disorders of
motor function, including
the book On tremor, palpitation, convulsion and
shivering. He distinguished between forms of shaking of the limb on the
basis of origin and appearance. The aged, he noted, exhibited tremor
because of a decline in their power to control motion of
their limbs. The key to overcoming tremor was to abolish the proximal
cause, but for the aged, this was impractical.
MEDIEVAL
HISTORY
 Paul
of Aigina (c625-c690) the
Byzantine Greek
physician, wrote the
medical encyclopedia "Medical
Compendium in Seven Books". For many years in the
Byzantine Empire, this work contained the
sum of all
Western medical knowledge and was
unrivaled in its accuracy and completeness. Paul of Aegina noted in his
work On trembling that tremor was characteristic of alcoholism and what
Mettler interpreted as "senile paralysis agitans". Paul
of Aigina (c625-c690) the
Byzantine Greek
physician, wrote the
medical encyclopedia "Medical
Compendium in Seven Books". For many years in the
Byzantine Empire, this work contained the
sum of all
Western medical knowledge and was
unrivaled in its accuracy and completeness. Paul of Aegina noted in his
work On trembling that tremor was characteristic of alcoholism and what
Mettler interpreted as "senile paralysis agitans".
 An
ancient Syrian medical text listed for nervous
diseases a complex unguent for "pains in the excretory organs and in the
joints, and in cases of gout and palsy, and for those who have the
tremors, and for all the pains which take place in the nerves". It
consists of thirty-five components, including frankincense, rosemary,
several types of cypress, cardamom, peppercorns, myrrh, mandragora and
frogs. It was to rubbed on the paralysed or rigid limb. An
ancient Syrian medical text listed for nervous
diseases a complex unguent for "pains in the excretory organs and in the
joints, and in cases of gout and palsy, and for those who have the
tremors, and for all the pains which take place in the nerves". It
consists of thirty-five components, including frankincense, rosemary,
several types of cypress, cardamom, peppercorns, myrrh, mandragora and
frogs. It was to rubbed on the paralysed or rigid limb.
 Ibn Sina
(c980-1037), the Persian polymath and foremost physician of his time
discussed the various forms of motor unrest
in his chapter on nervous disorders in the "Canon of Medicine". The
description of tremor is not unexpectedly similar to that of Galen, as it
was based on previous works including that of Galen. A range of measures
are proposed according to the cause of the disorder. Bathing in sea-water
or mineral baths (nitrate, arsenic, asphalt, sulphur) was recommended,
as was the ever popular evacuation; composite preparations including made
from the excretion of the anal gland of the beaver mixed with honey and cold oil, to which pills formed
from rue (Ruta graveolens) and scolopendrium (Scolopendrium vulgare;
hart's tongue). Ibn Sina
(c980-1037), the Persian polymath and foremost physician of his time
discussed the various forms of motor unrest
in his chapter on nervous disorders in the "Canon of Medicine". The
description of tremor is not unexpectedly similar to that of Galen, as it
was based on previous works including that of Galen. A range of measures
are proposed according to the cause of the disorder. Bathing in sea-water
or mineral baths (nitrate, arsenic, asphalt, sulphur) was recommended,
as was the ever popular evacuation; composite preparations including made
from the excretion of the anal gland of the beaver mixed with honey and cold oil, to which pills formed
from rue (Ruta graveolens) and scolopendrium (Scolopendrium vulgare;
hart's tongue).
SIXTEENTH CENTURY

|
The
Italian artist, engineer and scientist Leonardo da Vinci (1452-1519) also
studied anatomy, physiology and medicine. Leonardo da Vinci kept secret notebooks
in which he wrote and sketched his ideas and observations. He saw people
whose symptoms coincided with the tremors seen in Parkinson's Disease.
Leonardo wrote in his notebooks that "you will see.....those who.....move
their trembling parts, such as their heads or hands without permission of
the soul; (the) soul with all its forces cannot prevent these parts from
trembling." |
| |
|
 |
There are examples of references to the symptoms of Parkinson's
Disease in the plays of the English playwright William Shakespeare
(1564-1616). There is a reference to shaking palsy in the second
part of his historical play Henry VI, during an exchange between
Dick and Say. Say explains to Dick that it is shaking palsy rather
than fear that was causing his shaking. Dick asks Say : "Why dost
thou quiver, man ?" Say responds : "The palsy, and not fear,
provokes me." Shaking palsy was the old name for Parkinson's
Disease symptoms.
|
| |
|
 |
John Gerard (1545-1611/12)
was an
English
botanist famous for his
herbal garden. He studied medicine and
travelled widely as a ship's
surgeon. In
1597, he published a list of plants
cultivated in his
garden at
Holborn. It was basically a translation
of a 1583 Latin herbal illustrated. he writes of Sage
that it "strengthneth the sinewes, restoreth health to those that have the
palsie upon a moist cause, takes away shaking or trembling of the
members". He also mentioned cabbage, pellitory and mugwort for treating
trembling of the sinews. |
SEVENTEENTH CENTURY
 |
Nicholas
Culpeper (1616-1654) was an English botanist, herbalist, physician and
astrologer. In his book
Complete Herbal he suggests sage
for "sinews, troubled with palsy and cramp". Amongst other
plant remedies Culpepper suggested for palsy and trembling were
bilberries, briony (called "English mandrake"), and mistletoe. In his
Pharmacopoeia Londinensis, a variety
of substances were claimed to be useful in the
treatment of "palsies", the "dead
palsy", and "tremblings". These included "oil of winged ants" and
preparations including earthworms. |
| |
|
 |
The
writer and antiquary, John Aubrey (1626-1697) wrote a biography of the
philosopher Thomas
Hobbes (1588-1679) titled "Life of Mr Thomas Hobbes of Malmesbury".
In it, he used the
term "Shaking
Palsey" in his description of the progressive disability that had afflicted Thomas Hobbes.
John Aubrey wrote
of Thomas Hobbes that he "had the shaking Palsey in his hands.....and has grown upon him in degrees", and that
".....Mr Hobbs wase for severall yeares before he died so Paralyticall
that he wase scarce able to write his name". |
| |
|
 |
The
Hungarian doctor Ferenc P�pai P�riz (1649-1716) described in 1690 in his medical text Pax Corporis all four cardinal signs
of Parkinson's Disease :
tremor, bradykinesia, rigor and postural instability. This was the first
time that all the main symptoms of Parkinson's Disease have been formally
described. The book was only published in Hungarian, which has resulted in his description of
Parkinson's Disease being ignored in the medical literature in favour of
later descriptions of Parkinson's Disease wrongly being claimed to be the
first.
|
EIGHTEENTH CENTURY
 |
George Cheyne
(1671-1743) was a Scottish physician, psychologist, philosopher and
mathematician. It is possible to interpret
a disorder described in chapter XII of his The English Malady (1734) as
parkinsonian. The subject of his discussion is the vaguely defined
"Palsy", or "Paralytick Symptoms". "Palsy" was then defined as "a disease
wherein the body, or some of its members lose their motion, and sometimes
their sensation of feeling. The disease is never acute, often tedious, and
in old people, almost incurable. |
| |
|
 |
Francois Boissier
de Sauvages de la Croix (1706-1767) provided one of the clearest
descriptions of a parkinsonism-like condition in 1763. He spoke of a
condition that he named "sclerotyrbe festinans" in which decreased
muscular flexibility led to difficulties in the initiation of walking.
Both of the cases he observed were in elderly people. His observations,
along with those of Jerome David Gaubius
(1705-1780) and Franciscus de la Bo� (1614-1672)
were subsequently cited by James Parkinson. |
| |
|
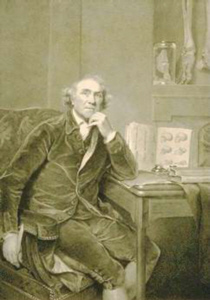 |
John
Hunter (1728-1793) was a distinguished Scottish surgeon. In his Croonian
lecture in 1776, John Hunter gave a description of Lord L. that was
similar to paralysis agitans. He wrote that "Lord L's hands are almost
perpetually in motion, and he never feels the sensation in them of being
tired. When he is asleep his hands, &c., are perfectly at rest; but when
he wakes in a little time they begin to move". It has been suggested that
James Parkinson may have attended this lecture. |
james parkinson
 Parkinson's
disease was first formally described in modern times in
"An Essay on the
Shaking Palsy," published
in 1817 by a London physician named
James Parkinson (1755-1824). James Parkinson
described the medical
history of six
individuals in London who had symptoms of the disease that eventually bore his name.
Unusually for such a description, he did not actually examine all these patients
himself but observed them on daily walks.
The purpose of his essay was to
document the symptoms of the medical disorder, which he described as
"Involuntary tremulous motion, with lessened muscular power, in parts not in
action and even when supported; with a propensity to bend the trunk
forwards, and to pass from a walking to a running pace : the senses and
intellect being uninjured." Parkinson's
disease was first formally described in modern times in
"An Essay on the
Shaking Palsy," published
in 1817 by a London physician named
James Parkinson (1755-1824). James Parkinson
described the medical
history of six
individuals in London who had symptoms of the disease that eventually bore his name.
Unusually for such a description, he did not actually examine all these patients
himself but observed them on daily walks.
The purpose of his essay was to
document the symptoms of the medical disorder, which he described as
"Involuntary tremulous motion, with lessened muscular power, in parts not in
action and even when supported; with a propensity to bend the trunk
forwards, and to pass from a walking to a running pace : the senses and
intellect being uninjured."
THE FIRST CLAIMED CURE
 English physician John
Elliotson (1791-1868) published pamphlets concerning the disorder from
1827 to 1831 in the Lancet, which largely consisted of case reports. Amongst his
preferred methods of treatment were bleeding, induction and maintenance of
pus building, cauterization, purging, low diet and mercurialization,
silver nitrate, arsenic, zinc sulphate, copper compounds, and the
administration of iron as a tonic with some porter, which is a kind of
dark beer. Elliotson made the first known claimed cure. He suggested that many young patients could be
cured using the carbonate of iron. On another
occasion, he reported that the �disease instantly and permanently gave
way� when he treated with iron a patient who had proved resistant to all
other forms of therapy. This was well over a century before iron was found
to be essential for the formation of L-dopa. English physician John
Elliotson (1791-1868) published pamphlets concerning the disorder from
1827 to 1831 in the Lancet, which largely consisted of case reports. Amongst his
preferred methods of treatment were bleeding, induction and maintenance of
pus building, cauterization, purging, low diet and mercurialization,
silver nitrate, arsenic, zinc sulphate, copper compounds, and the
administration of iron as a tonic with some porter, which is a kind of
dark beer. Elliotson made the first known claimed cure. He suggested that many young patients could be
cured using the carbonate of iron. On another
occasion, he reported that the �disease instantly and permanently gave
way� when he treated with iron a patient who had proved resistant to all
other forms of therapy. This was well over a century before iron was found
to be essential for the formation of L-dopa.
The first named patient
 Wilhelm von Humboldt (1767-1835), a
philosopher and diplomat, described in his letters from 1828 until his
death in 1835, his own medical history,
which gave a more complete description of the symptoms of Parkinson's Disease than had James Parkinson. They included resting tremor
and especially problems in writing, called by him "a special clumsiness"
that he attributed to a disturbance in executing rapid complex movements.
In addition to lucidly describing akinesia, he was also the first to
describe micrographia. He furthermore noticed his typical parkinsonian
posture. There were incidental references in the following decades to what
may (or may not) have been some of the symptoms of Parkinson�s Disease by
Toulmouche (1833), Hall (1836, 1841), Elliotson (1839), Romberg (1846). However, the syndrome remained hardly known. Wilhelm von Humboldt (1767-1835), a
philosopher and diplomat, described in his letters from 1828 until his
death in 1835, his own medical history,
which gave a more complete description of the symptoms of Parkinson's Disease than had James Parkinson. They included resting tremor
and especially problems in writing, called by him "a special clumsiness"
that he attributed to a disturbance in executing rapid complex movements.
In addition to lucidly describing akinesia, he was also the first to
describe micrographia. He furthermore noticed his typical parkinsonian
posture. There were incidental references in the following decades to what
may (or may not) have been some of the symptoms of Parkinson�s Disease by
Toulmouche (1833), Hall (1836, 1841), Elliotson (1839), Romberg (1846). However, the syndrome remained hardly known.
The naming of Parkinson's Disease
It was not until 1861 and 1862 that
Jean-Martin Charcot (1825-1893) with Alfred Vulpian (1826-1887) added
more symptoms to James Parkinson's clinical description, and
then subsequently confirmed James Parkinson's place in medical history by
attaching the name Parkinson's Disease to the syndrome.
 Charcot added to the list of symptoms the mask face, various forms of
contractions of hands and feet, akathesia as well as rigidity. It was only after Charcot gave a clinical lesson
in 1868 that the difference became clear (Charcot, 1868). In 1867 Charcot
introduced a treatment with the alkaloid drug hyoscine (or scopolamine)
derived from the Datura plant, which was used until the advent of L-Dopa a century later. In 1876 Charcot described a patient suffering from
Parkinson's disease in the absence of tremor, while rigidity was present. In
this case there was no paralysis, so Charcot rejected the term paralysis
agitans. Instead he suggested that the disease be referred to in future as
Parkinson's disease. Charcot added to the list of symptoms the mask face, various forms of
contractions of hands and feet, akathesia as well as rigidity. It was only after Charcot gave a clinical lesson
in 1868 that the difference became clear (Charcot, 1868). In 1867 Charcot
introduced a treatment with the alkaloid drug hyoscine (or scopolamine)
derived from the Datura plant, which was used until the advent of L-Dopa a century later. In 1876 Charcot described a patient suffering from
Parkinson's disease in the absence of tremor, while rigidity was present. In
this case there was no paralysis, so Charcot rejected the term paralysis
agitans. Instead he suggested that the disease be referred to in future as
Parkinson's disease.
THE FIRST KNOWN
DEPICTIONS OF PARKINSON'S DISEASE
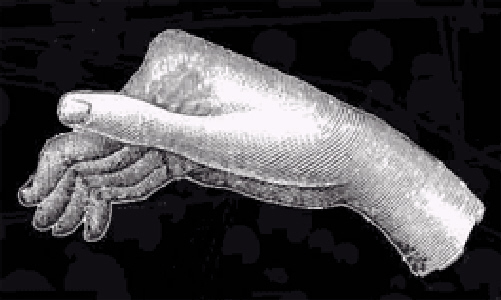
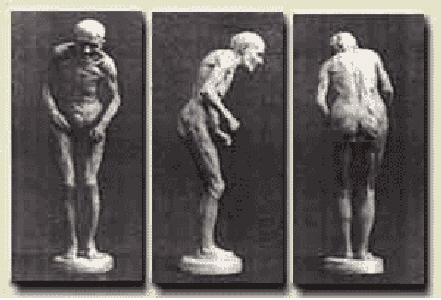
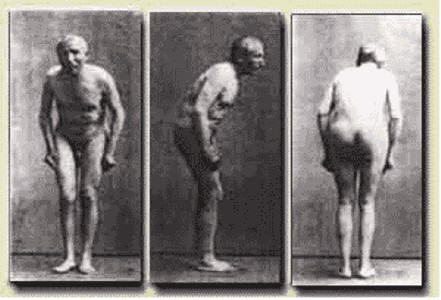
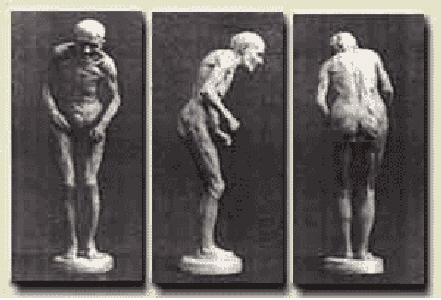
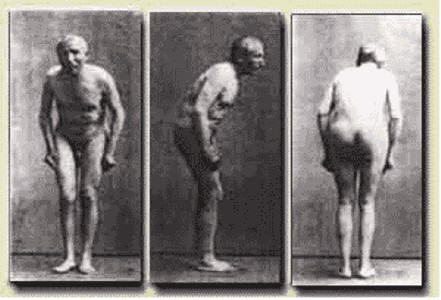
Paul Marie Louis
Pierre Richer (1849-1933) was a French anatomist, physiologist, sculptor and
anatomical artist. Paul Richer was an assistant to Jean-Martin Charcot at
the Salp�tri�re. In 1880, Jean-Marie Charcot completed a full clinical
description of Parkinson's Disease. The symptoms were depicted by Paul
Richer in drawings and a statuette of people with Parkinson's Disease.
Along with a photograph, these
are the first known depictions of Parkinson's Disease.
THE USE OF
ELECTROTHERAPY
In 1868
French doctor Guillame Benjamin-Amand Duchenne
(1806-1875),
had reported a case in which he had cured paralysis agitans by application
of galvanism.
Duchenne had
popularized the
use of electrical means with his 1855 publication "On localized
electrification, and on its application to pathology
and
therapy".
 Irish physician
U.S.L.Butler also claimed in 1869 that it cured a patient of paralysis
agitans.
Hughlings Jackson, and William Gowers in
1893, who also tried it in paralysis agitans, were unstinting in their
deprecation of the practice as "useless".
Despite this, electrical stimulation
in Parkinson�s disease continued to be used for decades more. In the 1924
edition of his handbook on electrotherapy, Toby Cohn commented that
"remarkable results could not be expected", and that what benefits he had
seen were largely psychological. In his 1941 review of the "modern treatment
of parkinsonism", Critchley specifically warned against electricity and
other spurious claims of curing the disease. Irish physician
U.S.L.Butler also claimed in 1869 that it cured a patient of paralysis
agitans.
Hughlings Jackson, and William Gowers in
1893, who also tried it in paralysis agitans, were unstinting in their
deprecation of the practice as "useless".
Despite this, electrical stimulation
in Parkinson�s disease continued to be used for decades more. In the 1924
edition of his handbook on electrotherapy, Toby Cohn commented that
"remarkable results could not be expected", and that what benefits he had
seen were largely psychological. In his 1941 review of the "modern treatment
of parkinsonism", Critchley specifically warned against electricity and
other spurious claims of curing the disease.
Expanding the known symptoms
After Charcot
initiated the research of incomplete forms of Parkinson's disease, rigidity
as a symptom grew in importance. In 1892 B�chet
made the remark that all symptoms of Parkinson's disease were secondary
to rigidity,
tremor being an
exception.
 Although Charcot and Parkinson pointed out that
patients are moving slowly and with difficulty, they did not see this as a
symptom in its own right. The slowness of movement was firstly taken into
account by Claveleira and it became a new element of the definition. Jaccoud referred to this symptom in 1873 as akinesia.
In 1886, the neurologist and artist, Sir William Richard Gowers, drew an
illustration in 1886 as part of his documentation of Parkinson's Disease.
Cruchet introduced the word bradykinesia and emphasized that this symptom
should be mentioned in any definition of Parkinson's
disease.
Jules
Froment, a French neurologist, contributed to the study of
parkinsonian rigidity during the 1920s. Although Charcot and Parkinson pointed out that
patients are moving slowly and with difficulty, they did not see this as a
symptom in its own right. The slowness of movement was firstly taken into
account by Claveleira and it became a new element of the definition. Jaccoud referred to this symptom in 1873 as akinesia.
In 1886, the neurologist and artist, Sir William Richard Gowers, drew an
illustration in 1886 as part of his documentation of Parkinson's Disease.
Cruchet introduced the word bradykinesia and emphasized that this symptom
should be mentioned in any definition of Parkinson's
disease.
Jules
Froment, a French neurologist, contributed to the study of
parkinsonian rigidity during the 1920s.
ENCEPHALITIS
LETHARGICA
In 1915,
epidemics of Encephalitis Lethargica broke out around the world. It was
first described in 1917 by the Austrian neurologist Constantin von Economo.
It started off as an influenza like fever, and then developed in to
symptoms such as headache, depression, delirium, confusion, motor
disturbances, psychosis and stupor.
 Its
symptoms were thought to encompass
almost anything imaginable. Encephalitis Lethargica could cause death in a
short period, or a type of sleep that might last days, weeks or months,
but could also cause insomnia. Many of those that survived developed Postencephalitic Parkinsonism. Encephalitis Lethargica consequently led to
a huge increase in the number of people with Parkinsonism. In the 1920's,
the majority of Parkinsonian patients had Postencephalitic Parkinsonism. Its
symptoms were thought to encompass
almost anything imaginable. Encephalitis Lethargica could cause death in a
short period, or a type of sleep that might last days, weeks or months,
but could also cause insomnia. Many of those that survived developed Postencephalitic Parkinsonism. Encephalitis Lethargica consequently led to
a huge increase in the number of people with Parkinsonism. In the 1920's,
the majority of Parkinsonian patients had Postencephalitic Parkinsonism.
THE USE OF
ALKALOIDS
The first
widespread use of the alkaloid atropine was in the 1920's. High dose
atropine therapy dominated in the first half of the 1930's, achieving
significant results, but it was accompanied by serious side effects. In
1926, the Bulgarian Ivan Raeff introduced in to the treatment of post
encephalitic Parkinsonism what was later called the "Bulgarian treatment",
which was white wine extract of the belladonna root. It was the belladonna
root that was the effective part. The alkaloid content of the extract
included varying amounts of hyoscyamine, atropine and, in lesser
quantities, scopolamine and belladonnine. By the beginning of the 1940's
most patients were being treated using belladonna alkaloids.
THE USE OF
NEUROSURGERY
The first
specific attempt to treat Parkinsonism surgically was reported by Leriche
in 1912, via section of the posterior roots. The method relieved tremor or
rigidity. Improvements in tremor were subsequently
achieved by cortectomy, but often at the price of other functional losses.
Cordotomy was directed against unilateral tremor and rigidity, and
associated with fewer side effects. Meyers reported in 1951 that
sectioning of pallidofugal fibres achieved the best results for relieving
tremor and rigidity, but most surgeons chose to undertake a more direct
attack on the pallidum, with equal success and a lower fatality rate. The thalamus gradually
became the preferred target, as the impact on tremor was greater and the
operation was safer. After a sharp decline in stereotactic surgery,
thalamotomy was revived in the 1970's for tremor that was not
helped by L-dopa.
NEW SYNTHETIC
DRUGS
During the
1950's, synthetic drugs became the main methods of treating Parkinson's
Disease. Due to their side effects and limited efficacy, the plant derived
treatments were almost completely replaced by these synthetic drugs. The
main type of drugs used were anti-cholinergics because of their ability to
reduce muscle contraction. The most
widely used of them
was Benzhexol HCl, which had anti-cholinergic activity. It was marketed as
Artane in the U.S.A.. It was then the primary choice for treating
Parkinson's Disease. To a lesser extent
anti- histaminergics were also used for Parkinson's Disease. They lessened
the effect of allergic reactions, but also reduced muscle contraction.
Anti-histaminergic drugs were sold commercially, but only two of them,
diphenhydramine (Benadryl) and phenindamine (Theophorin), were widely used
in Parkinson's Disease.
The biochemistry of L-dopa
 The underlying
biochemical changes in the brain were identified in the 1950s, due largely
to the work of Swedish scientist Arvid Carlsson (born 1923). In the 1950s,
Arvid Carlsson demonstrated that dopamine was a neurotransmitter in the brain and
not just a precursor for norepinephrine, as had been previously believed. He
developed a method for measuring the amount of dopamine in brain tissues and
found that dopamine levels in the basal ganglia, a brain area important for
movement, were particularly high. He then showed that giving animals the
drug reserpine caused a decrease in dopamine levels and a loss of movement
control. These effects were similar to the symptoms of Parkinson's disease.
Arvid Carlsson subsequently won the Nobel Prize in Physiology or Medicine in
2000 along with co-recipients Eric Kandel and Paul Greengard. The underlying
biochemical changes in the brain were identified in the 1950s, due largely
to the work of Swedish scientist Arvid Carlsson (born 1923). In the 1950s,
Arvid Carlsson demonstrated that dopamine was a neurotransmitter in the brain and
not just a precursor for norepinephrine, as had been previously believed. He
developed a method for measuring the amount of dopamine in brain tissues and
found that dopamine levels in the basal ganglia, a brain area important for
movement, were particularly high. He then showed that giving animals the
drug reserpine caused a decrease in dopamine levels and a loss of movement
control. These effects were similar to the symptoms of Parkinson's disease.
Arvid Carlsson subsequently won the Nobel Prize in Physiology or Medicine in
2000 along with co-recipients Eric Kandel and Paul Greengard.
The therapeutic
use L-dopa
 These findings led other doctors
to try L-Dopa with human Parkinson's patients and found it to alleviate some
of the symptoms in the early stages of Parkinson's. Unlike dopamine, its
precursor L-Dopa could pass the blood brain barrier.
The validity of the approach was shown by the transient benefit seen after
injection of L-dopa.
However, it was not of practical
value as a treatment because of the severe toxicity associated with the
injection. At this point,
George C. Cotzias
(1918-1977)
made
a critical observation that converted the transient response into a
successful, large scale treatment. By starting with very small doses, given orally every two hours under continued observation, and
gradually increasing the dose he was able to stabilize patients on large
enough doses to cause a dramatic remission of their symptoms. Its findings
were
published in 1968. These findings led other doctors
to try L-Dopa with human Parkinson's patients and found it to alleviate some
of the symptoms in the early stages of Parkinson's. Unlike dopamine, its
precursor L-Dopa could pass the blood brain barrier.
The validity of the approach was shown by the transient benefit seen after
injection of L-dopa.
However, it was not of practical
value as a treatment because of the severe toxicity associated with the
injection. At this point,
George C. Cotzias
(1918-1977)
made
a critical observation that converted the transient response into a
successful, large scale treatment. By starting with very small doses, given orally every two hours under continued observation, and
gradually increasing the dose he was able to stabilize patients on large
enough doses to cause a dramatic remission of their symptoms. Its findings
were
published in 1968.
SINEMET AND
MADOPAR
There
were efforts to improve on the administration of L-dopa in order to lessen
its side effects. Dopa decarboxylase inhibitors reduced the metabolism of
L-dopa. L-dopa combined with the decarboxylase inhibitor carbidopa was
commercially launched in 1972 as Sinemet. Carbidopa made the product more
effective by delaying the conversion of L-dopa into dopamine until the
drug passed into the brain. The product was improved in 1991 when approval
was given for Sinemet CR, which is a controlled release version. The combination of L-dopa with the decarboxylase inhibitor
benserazide was commercially launched by Hoffmann-LaRoche in 1973 as
Madopar. It was eventually produced in a controlled release version
called Madopar CR.
MAO INHIBITORS
During
the 1970's, MAO inhibitors were introduced in order to prolong the effect
of L-dopa by delaying its breakdown. By inhibiting Monoamine Oxidase, MAO
inhibitors were shown to be able to raise dopamine levels, but the side
effects were severe. In 1968 it was shown that there were two MAO enzymes,
MAO-A and MAO-B. Inhibition of MAO-B was suitable for Parkinson's Disease.
The inhibition of MAO-B was not subject to the same risks as MAO
generally. The most suitable drug for use as a MAO-B inhibitor, called at
the time E-250, was launched commercially in 1977. Its use gradually
spread to other countries, but it was not approved in the U.S.A. until
1989. It came to be known as Selegiline. Since then, other MAO-B
inhibitors such as Rasagiline have been used in Parkinson's Disease.
DOPAMINE AGONISTS
Despite L-dopa
initially being seen as a major breakthrough, as many as 25% of people
taking L-dopa did not respond to it. Other people were being caused
widespread side effects due to using it, including dsykinesia.
Consequently, directly stimulating the dopamine receptors using dopamine
agonists appeared to some to be a better
option. Cotzias
demonstrated
efficacy using apomorphine in the treatment of Parkinsonism. When used
alongside L-dopa, its effects appeared to be additive. In 1974, another
dopamine agonist, bromocriptine, for the treatment of Parkinson's Disease,
was introduced. Following the initial success of bromocriptine, other
dopamine agonists were clinically trialled, including cabergoline, lisuride, pergolide, pramipexole, ropinirole, and
eventually, rotigotine. However, all of the dopamine agonists caused side
effects of their own.
FROM 2000 ONWARDS
From 2000
onwards, L-dopa primarily as Sinemet and Madopar was already being widely
used in the treatment of Parkinson's Disease, as were MAO-B inhibitors and
dopamine agonists. Even more variants of each or them were being used,
assessed or introduced. The primary new means of treating Parkinson's
Disease were different formats of L-dopa, including Rytary and
Numient, COMT
inhibitors, and Deep Brain Stimulation, which is quite an effective means
of surgery. Although Stem cell surgery had been claimed capable of curing
Parkinson's Disease it subsequently failed all its clinical trials.
Besides these methods there was a proliferation of new approaches to the
treatment of Parkinson's Disease that have become progressively more
diverse, but scientifically unsound.
After
thousands of years of describing and treating Parkinson's Disease, and
despite the enormous resources used in developing new treatments, each
method of treating Parkinson's Disease has been found to have serious
inadequacies. The ultimate therapy, one that was able to rid symptoms
without side effects is still to be revealed.
|
.gif)
.gif)














 Charcot added to the list of symptoms the mask face, various forms of
contractions of hands and feet, akathesia as well as rigidity. It was only after Charcot gave a clinical lesson
in 1868 that the difference became clear (Charcot, 1868). In 1867 Charcot
introduced a treatment with the alkaloid drug hyoscine (or scopolamine)
derived from the Datura plant, which was used until the advent of L-Dopa a century later. In 1876 Charcot described a patient suffering from
Parkinson's disease in the absence of tremor, while rigidity was present. In
this case there was no paralysis, so Charcot rejected the term paralysis
agitans. Instead he suggested that the disease be referred to in future as
Parkinson's disease.
Charcot added to the list of symptoms the mask face, various forms of
contractions of hands and feet, akathesia as well as rigidity. It was only after Charcot gave a clinical lesson
in 1868 that the difference became clear (Charcot, 1868). In 1867 Charcot
introduced a treatment with the alkaloid drug hyoscine (or scopolamine)
derived from the Datura plant, which was used until the advent of L-Dopa a century later. In 1876 Charcot described a patient suffering from
Parkinson's disease in the absence of tremor, while rigidity was present. In
this case there was no paralysis, so Charcot rejected the term paralysis
agitans. Instead he suggested that the disease be referred to in future as
Parkinson's disease.

 Although Charcot and Parkinson pointed out that
patients are moving slowly and with difficulty, they did not see this as a
symptom in its own right. The slowness of movement was firstly taken into
account by Claveleira and it became a new element of the definition. Jaccoud referred to this symptom in 1873 as akinesia.
In 1886, the neurologist and artist, Sir William Richard Gowers, drew an
illustration in 1886 as part of his documentation of Parkinson's Disease.
Cruchet introduced the word bradykinesia and emphasized that this symptom
should be mentioned in any definition of Parkinson's
disease.
Although Charcot and Parkinson pointed out that
patients are moving slowly and with difficulty, they did not see this as a
symptom in its own right. The slowness of movement was firstly taken into
account by Claveleira and it became a new element of the definition. Jaccoud referred to this symptom in 1873 as akinesia.
In 1886, the neurologist and artist, Sir William Richard Gowers, drew an
illustration in 1886 as part of his documentation of Parkinson's Disease.
Cruchet introduced the word bradykinesia and emphasized that this symptom
should be mentioned in any definition of Parkinson's
disease.  Its
symptoms were thought to encompass
almost anything imaginable. Encephalitis Lethargica could cause death in a
short period, or a type of sleep that might last days, weeks or months,
but could also cause insomnia. Many of those that survived developed Postencephalitic Parkinsonism. Encephalitis Lethargica consequently led to
a huge increase in the number of people with Parkinsonism. In the 1920's,
the majority of Parkinsonian patients had Postencephalitic Parkinsonism.
Its
symptoms were thought to encompass
almost anything imaginable. Encephalitis Lethargica could cause death in a
short period, or a type of sleep that might last days, weeks or months,
but could also cause insomnia. Many of those that survived developed Postencephalitic Parkinsonism. Encephalitis Lethargica consequently led to
a huge increase in the number of people with Parkinsonism. In the 1920's,
the majority of Parkinsonian patients had Postencephalitic Parkinsonism.